By Silent
•
January 7, 2026
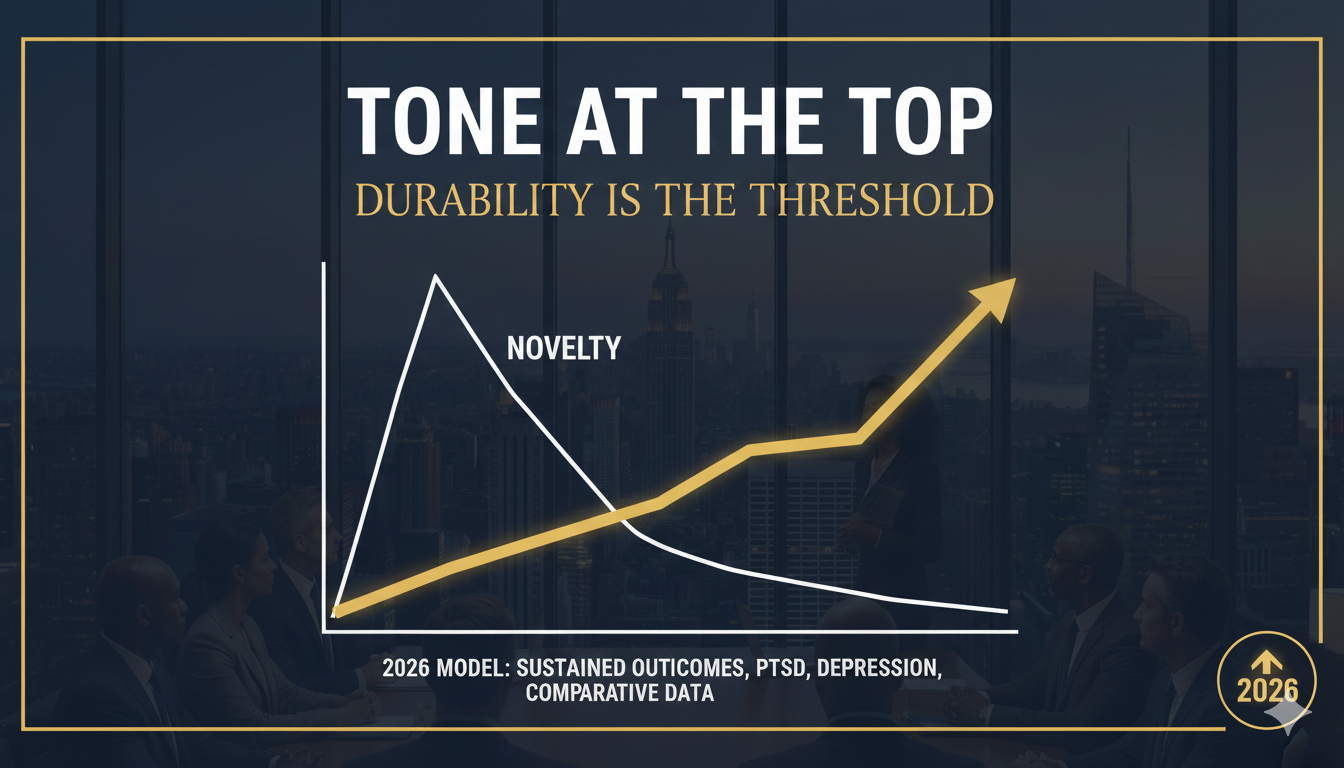
Thesis: Oregon refined service centers. Colorado designed healing centers. 2026 will reveal which model actually scales with integrity . Top of Mind Policy debates often end too early. A bill passes. A framework launches. Headlines move on. But leaders know the truth: implementation is where intent is either honored—or quietly betrayed . As we head into 2026, two states offer a live case study in how access evolves after legalization energy fades. Oregon and Colorado are no longer asking whether access exists. They are confronting a harder question: What kind of access survives contact with reality? Their answers are diverging—and instructive. What Oregon taught us about operations Oregon’s early days were messy by design. The state moved fast, prioritized openness, and let the system reveal its own weak points. That phase is over. What’s emerged is an operationally disciplined model centered on service centers , and the refinements are telling. Training standards are tightening. Initial facilitator requirements left too much to interpretation. In response, Oregon has begun clarifying competencies—not just hours logged, but demonstrated skills in preparation, holding altered states, and post-session integration. This isn’t about credential inflation; it’s about reducing variance where vulnerability is high. Screening is no longer optional. Early narratives romanticized accessibility. Experience corrected that. Medical history, psychological readiness, medication interactions, and support systems are now treated as foundational—not barriers, but safeguards. Oregon learned the hard way that access without screening creates downstream harm that no amount of integration can fully repair. Integration is becoming non-negotiable. Perhaps the most important shift: integration is no longer framed as “nice to have.” Service centers are increasingly required to demonstrate how insights are supported over time—through structured sessions, referrals, and continuity of care. Oregon’s model is converging on a simple truth executives recognize immediately: outcomes decay without follow-through . Operationally, Oregon has become quieter, slower, and more serious. That’s not a retreat. It’s maturation. What Colorado emphasized from the start Colorado took a different path—not faster, but broader. Where Oregon optimized delivery, Colorado focused on designing the ecosystem itself . Equity licensing is structural, not symbolic. Colorado embedded equity considerations directly into licensing frameworks, aiming to prevent early capture by well-capitalized operators. This wasn’t perfect, but it sent a clear signal: access is not just about who receives services, but who is allowed to provide them. Indigenous consultation shaped the model. Rather than treating Indigenous voices as ceremonial, Colorado engaged them as stakeholders in governance conversations. That didn’t resolve every tension, but it shifted the tone. Healing was framed less as a transaction and more as a responsibility carried across generations. Outcomes data was prioritized early. Colorado placed emphasis on what gets measured—not just utilization, but impact. This includes safety events, participant-reported outcomes, and longer-term indicators of well-being. The state implicitly acknowledged a leadership axiom too often ignored: what you don’t measure, you don’t really care about . Colorado’s approach is less operationally tight today—but culturally and ethically ambitious. The 2026 friction points no one can avoid As both models collide with scale, three friction points are becoming unavoidable. Affordability. High-touch care is expensive. Training, screening, supervision, and integration all cost money. Without intervention, access risks drifting toward those who can already afford private alternatives. Both states face pressure to reconcile integrity with affordability—without diluting either. Workforce capacity. Facilitators, clinicians, supervisors, and integration specialists are finite. Scaling demand without burning out the workforce is not a regulatory issue; it’s a leadership one. Oregon’s tighter standards and Colorado’s broader inclusion both strain the same human bottleneck. Rural access. Urban centers benefit first. That’s predictable—and unacceptable if equity is more than rhetoric. Rural access challenges transportation, workforce distribution, and cultural relevance. Neither state has cracked this yet. 2026 will force the issue. Cross-pollination: what each state should steal from the other If leaders are paying attention, the answer isn’t choosing one model. It’s selective theft . What Oregon should steal from Colorado: · Formal equity metrics tied to licensing outcomes · Required outcomes reporting beyond safety compliance · Ongoing Indigenous and community consultation baked into governance What Colorado should steal from Oregon: · Clear, enforceable training standards · Mandatory screening protocols · Defined integration pathways with accountability This isn’t ideological blending. It’s operational wisdom. Strong systems borrow shamelessly. Closing: implementation is policy By 2026, the debate won’t be about access on paper. It will be about lived experience. Leaders should internalize this now: implementation is policy . Training standards shape safety. Screening determines who is harmed or helped. Integration defines whether insight becomes change or fades into memory. Frameworks don’t fail loudly. They fail quietly—through inconsistency, burnout, and unmeasured outcomes. Call to Action If you’re working in this space—clinician, operator, regulator, or funder—tell us what you believe should be measured. Not vanity metrics. Outcomes that actually matter. Because what we choose to measure in 2026 will decide which future of access we’re really building. Onward.